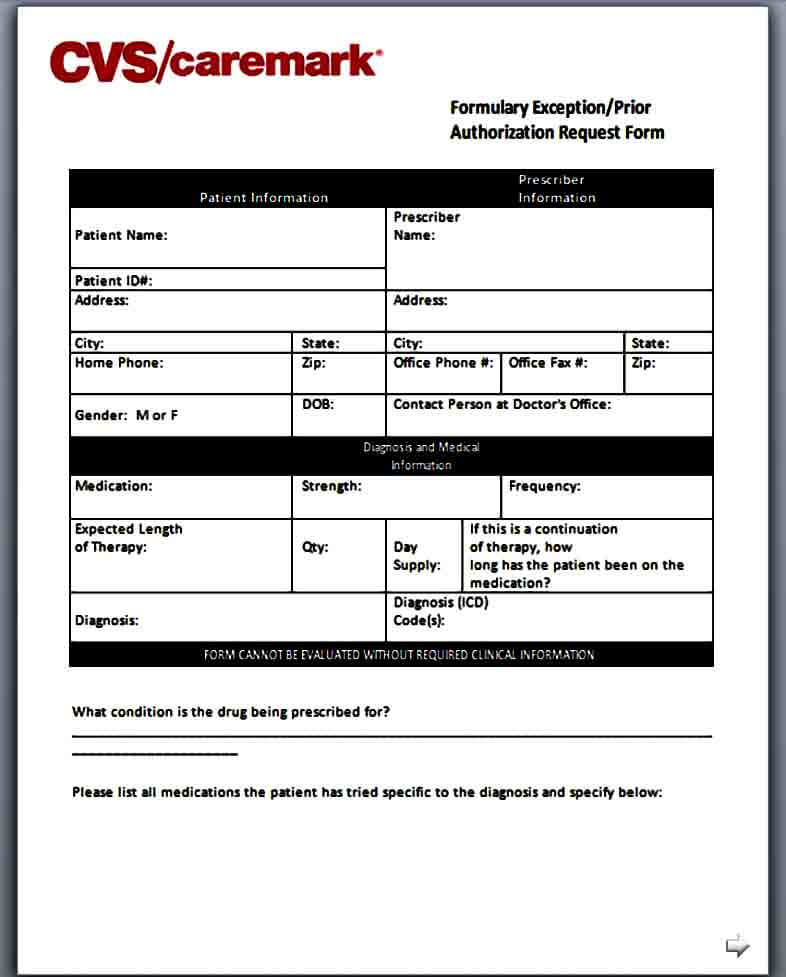
Cvs Caremark Prior Authorization Appeal Form . prescription benefit plan may request additional information or clarification, if needed, to evaluate. requests that are subject to prior authorization (or any other utilization management requirement), may require. When a pa is needed for a prescription, the member will be asked to. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. Initial prior authorization with quantity limit. if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark. download and complete this form to request coverage for a medication that requires prior authorization.
from moussyusa.com
i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. download and complete this form to request coverage for a medication that requires prior authorization. prescription benefit plan may request additional information or clarification, if needed, to evaluate. Initial prior authorization with quantity limit. requests that are subject to prior authorization (or any other utilization management requirement), may require. When a pa is needed for a prescription, the member will be asked to. if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark.
Template Caremark Prior Authorization Form Mous Syusa
Cvs Caremark Prior Authorization Appeal Form When a pa is needed for a prescription, the member will be asked to. requests that are subject to prior authorization (or any other utilization management requirement), may require. Initial prior authorization with quantity limit. prescription benefit plan may request additional information or clarification, if needed, to evaluate. download and complete this form to request coverage for a medication that requires prior authorization. When a pa is needed for a prescription, the member will be asked to. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark.
From www.authorizationform.net
Cvs Pharmacy Prior Authorization Form Cvs Caremark Prior Authorization Appeal Form When a pa is needed for a prescription, the member will be asked to. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. Initial prior authorization with quantity limit. prescription benefit plan may request additional information or clarification, if needed, to evaluate. requests that are subject. Cvs Caremark Prior Authorization Appeal Form.
From www.formsbank.com
Plan Member Authorization Form Cvs/caremark printable pdf download Cvs Caremark Prior Authorization Appeal Form When a pa is needed for a prescription, the member will be asked to. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. Initial prior authorization with quantity limit. prescription benefit plan may request additional information or clarification, if needed, to evaluate. if the prescriber would. Cvs Caremark Prior Authorization Appeal Form.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form Cvs Caremark Prior Authorization Appeal Form if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark. prescription benefit plan may request additional information or clarification, if needed, to evaluate. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. download and complete this. Cvs Caremark Prior Authorization Appeal Form.
From www.pdffiller.com
Fillable Online HMSA Prior Authorization Request CVS Caremark Fax Cvs Caremark Prior Authorization Appeal Form if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark. Initial prior authorization with quantity limit. download and complete this form to request coverage for a medication that requires prior authorization. prescription benefit plan may request additional information or clarification, if needed, to evaluate. i further attest. Cvs Caremark Prior Authorization Appeal Form.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Appeal Form When a pa is needed for a prescription, the member will be asked to. Initial prior authorization with quantity limit. download and complete this form to request coverage for a medication that requires prior authorization. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. if the. Cvs Caremark Prior Authorization Appeal Form.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Authorization Appeal Form When a pa is needed for a prescription, the member will be asked to. Initial prior authorization with quantity limit. if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark. prescription benefit plan may request additional information or clarification, if needed, to evaluate. requests that are subject to. Cvs Caremark Prior Authorization Appeal Form.
From www.templateroller.com
Prior Authorization Request Form Cvs Caremark Fill Out, Sign Online Cvs Caremark Prior Authorization Appeal Form When a pa is needed for a prescription, the member will be asked to. requests that are subject to prior authorization (or any other utilization management requirement), may require. Initial prior authorization with quantity limit. if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark. prescription benefit plan. Cvs Caremark Prior Authorization Appeal Form.
From www.pdffiller.com
20212024 Form CVS Caremark 10637207A Fill Online, Printable, Fillable Cvs Caremark Prior Authorization Appeal Form download and complete this form to request coverage for a medication that requires prior authorization. Initial prior authorization with quantity limit. When a pa is needed for a prescription, the member will be asked to. if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark. requests that are. Cvs Caremark Prior Authorization Appeal Form.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Authorization Appeal Form if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark. download and complete this form to request coverage for a medication that requires prior authorization. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. When a pa. Cvs Caremark Prior Authorization Appeal Form.
From www.signnow.com
Cvs Caremark Appeal Form Edit & Share airSlate SignNow Cvs Caremark Prior Authorization Appeal Form When a pa is needed for a prescription, the member will be asked to. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. requests that are subject to prior authorization (or any other utilization management requirement), may require. download and complete this form to request coverage. Cvs Caremark Prior Authorization Appeal Form.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Authorization Appeal Form prescription benefit plan may request additional information or clarification, if needed, to evaluate. requests that are subject to prior authorization (or any other utilization management requirement), may require. Initial prior authorization with quantity limit. download and complete this form to request coverage for a medication that requires prior authorization. if the prescriber would like to discuss. Cvs Caremark Prior Authorization Appeal Form.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Appeal Form When a pa is needed for a prescription, the member will be asked to. download and complete this form to request coverage for a medication that requires prior authorization. prescription benefit plan may request additional information or clarification, if needed, to evaluate. Initial prior authorization with quantity limit. requests that are subject to prior authorization (or any. Cvs Caremark Prior Authorization Appeal Form.
From www.signnow.com
Cvs Caremark Appeal PDF 20032024 Form Fill Out and Sign Printable Cvs Caremark Prior Authorization Appeal Form if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the cvs/caremark. Initial prior authorization with quantity limit. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. download and complete this form to request coverage for a medication that. Cvs Caremark Prior Authorization Appeal Form.
From www.pdffiller.com
Fillable Online HMSA Prior Authorization Request CVS Caremark Cvs Caremark Prior Authorization Appeal Form Initial prior authorization with quantity limit. requests that are subject to prior authorization (or any other utilization management requirement), may require. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. download and complete this form to request coverage for a medication that requires prior authorization. When. Cvs Caremark Prior Authorization Appeal Form.
From www.formsbank.com
Caremark Prior Authorization Criteria Request Form printable pdf download Cvs Caremark Prior Authorization Appeal Form i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. When a pa is needed for a prescription, the member will be asked to. requests that are subject to prior authorization (or any other utilization management requirement), may require. download and complete this form to request coverage. Cvs Caremark Prior Authorization Appeal Form.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Authorization Appeal Form Initial prior authorization with quantity limit. i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. When a pa is needed for a prescription, the member will be asked to. requests that are subject to prior authorization (or any other utilization management requirement), may require. if the. Cvs Caremark Prior Authorization Appeal Form.
From www.pdffiller.com
Fillable Online Cvs caremark prior authorization form Fax Email Print Cvs Caremark Prior Authorization Appeal Form prescription benefit plan may request additional information or clarification, if needed, to evaluate. download and complete this form to request coverage for a medication that requires prior authorization. requests that are subject to prior authorization (or any other utilization management requirement), may require. if the prescriber would like to discuss a prior authorization determination with a. Cvs Caremark Prior Authorization Appeal Form.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Authorization Appeal Form i further attest that the information provided is accurate and true, and that documentation supporting this information is available for. Initial prior authorization with quantity limit. prescription benefit plan may request additional information or clarification, if needed, to evaluate. if the prescriber would like to discuss a prior authorization determination with a clinical peer, please contact the. Cvs Caremark Prior Authorization Appeal Form.